|
Use of Skin-Shock at the Judge Rotenberg Educational Center (JRC) |
SUCCESSFUL REDUCTION OF RITUALISTIC BEHAVIORS IN
A 36-YEAR-OLD WOMAN
WITH OBSESSIVE COMPULSIVE DISORDER WITH CONTINGENT SKIN SHOCK
Robert E. von Heyn, MaryEllen Kelley, and Matthew Israel.
Judge Rotenberg Educational Center
Canton, MA USA
Introduction
The Judge Rotenberg Educational Center operates day and residential programs for children and adults with behavior problems, including conduct disorders, emotional problems, brain injury or psychosis, autism and developmental disabilities. The basic approach taken in all of JRC's programs is the use of behavioral psychology and its various technological applications, such as behavioral education, programmed instruction, precision teaching, behavior modification, behavior therapy and behavioral counseling. From JRC's inception, its basic philosophy has always included the following principles: a willingness to accept students with the most difficult behavioral problems and a refusal to reject or expel any student because of the difficulty of his or her presenting behaviors; the use of a highly structured, consistent application of behavioral psychology to both the education and treatment of its students; a minimization of the use of psychotropic medication; and the use of the most effective behavioral education and treatment procedures available.
Methods
Participant
A 36-year-old woman who entered residential treatment following over 17 years of psychiatric hospitalizations associated with her severe Obsessive Compulsive Disorder participated in this single subject study. Excessive hand washing began when she was three and her repetitive behaviors escalated from then on. The ritualized behaviors associated with her disorder prevented her from performing even simple daily activities. If someone intervened while she was engaged in these ritualistic behaviors she became intensely violent. Many staff were injured as a result of her physical aggression. Many of her ritualistic behaviors, such as frequent hand washing and hair brushing, led to self-injury.
Treatment History
Available records indicate outpatient mental health treatment began when she was 12 and she left school when she was 15 when she began a series of hospitalizations. During the years of hospitalizations a myriad of pharmacological interventions had been used and included Xanax, Inderal, Depakene, Prozac, Folic Acid, Lithium, Ativan, Prolixin, Anafranil, Klonopin, Clozaril, Celexa, Cogentin, Risperdal, Trilafon, Klonopin, Thorazine, Mellarill, Zoloft, Trofanil, Trazadone, Loxitane, Orap, Benadryl, Dilantin, Corgard and Aventyl. Psychotherapy and behavioral plans were unsuccessful and records indicate that there was no change in her presentation after all of these years of treatment. In addition, Electro-Convulsive Shock Therapy and Cingulotomy were considered but rejected.
Apparatus
Contingent skin shock was delivered by a Graduated Electronic Decelerator (GED). Stimulus was 2-seconds in duration, at a 25% duty cycle with an average current of 15.5 mA RMS. Further detail can be found at www.effectivetreatment.org.
Procedure
Upon entering residential treatment, positive-only programming, mostly using multiple DRO contracts was conducted for the first 29 weeks. During this time, increasing educational, vocational and habilitative demands were placed on her as part of her treatment to maximize her ability to move to a less restrictive environment. Also during the initial 29 weeks she was weaned off Risperdal, Anafranil and Klonopin as these medications showed little or no effect on her problem behaviors. When it was concluded that the positive-only behavior program was not effective in decelerating her behaviors, the treatment was supplemented with court approved contingent skin shock for her aggressive, destructive, health dangerous, major disruptive and noncompliant behaviors. Initially ritualistic behaviors were treated with a token system and not with the GED. As almost all her behaviors in all environments were ritualized, it would not have been feasible to implement the GED at that time. After approximately two years, specific rituals were operationally defined, rate measured, and then treated with contingent skin shock. Following the successful reduction of each targeted ritualistic behavior, subsequent rituals were identified, measured and treated.
Results and Discussion
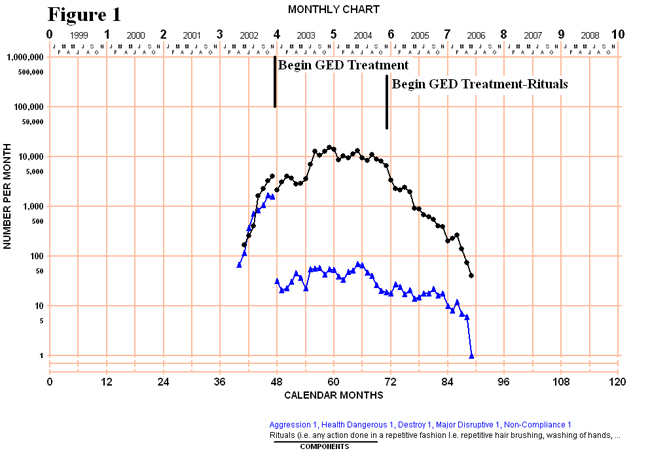
Figure 1 depicts the monthly total number of GED targeted behaviors (blue) and the monthly total number of ritualistic behaviors (black), before and after GED treatment began. Both categories of behaviors were accelerating during the pre-GED phase, which was likely a result of the increasing demands at JRC, such as requirements to complete chores or other activities that were not previously required. When GED was introduced, the data showed an immediate reduction of her aggressive, self-injurious, disruptive, destructive and noncompliant behaviors. These behaviors jumped down from a total of more than 1,500 a month to generally less than 50. However, there was no generalization of treatment to her ritualistic behaviors which continued to rise. It is likely that with her dangerous and disruptive behaviors occurring less frequently, she had more opportunity to exhibit ritualistic behaviors. Over time her dangerous and disruptive behaviors continued to decelerate and the last data point on the chart was under 10 in a month. The second phase line indicates when GED treatment began for some of her ritualistic behaviors. When a specific ritual was identified, it was moved out of the category depicted in Figure 1 and, therefore, none of the rituals depicted in that chart received GED treatment.
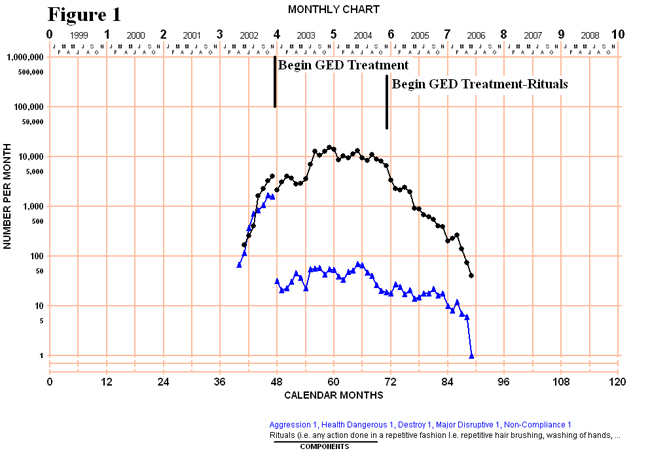
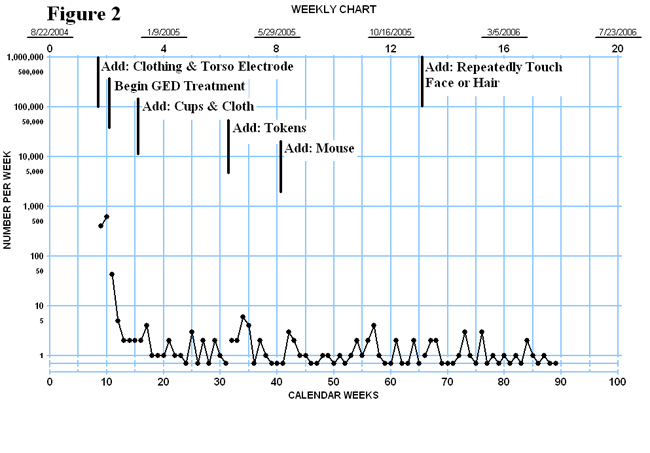
Figure 2 depicts the weekly the frequency of all of her ritualistic behaviors that received GED treatment. The first phase line shows the beginning of baseline of clothing related rituals. During the 19 days these behaviors were recorded but not treated, she exhibited more than 1,000 of these behaviors. Following treatment, she averaged less than 3 per week. The rest of the chart presents only data of ritualistic behaviors that were treated with GED. Figure 2 contains the addition of 5 high frequency ritualistic behaviors that were reduced to a median of only once per week over an 18 month period. Baseline data for the ritualistic behaviors treated with the GED are depicted in Figures 3 and 4.
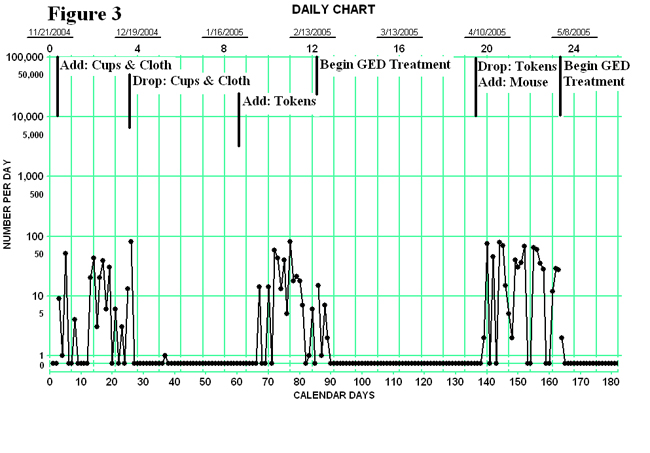
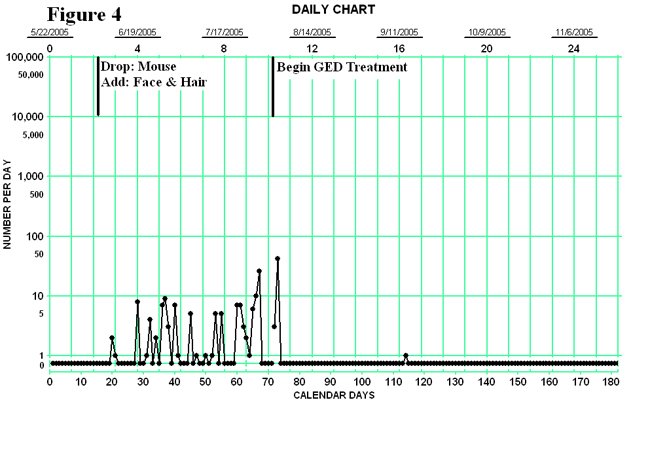
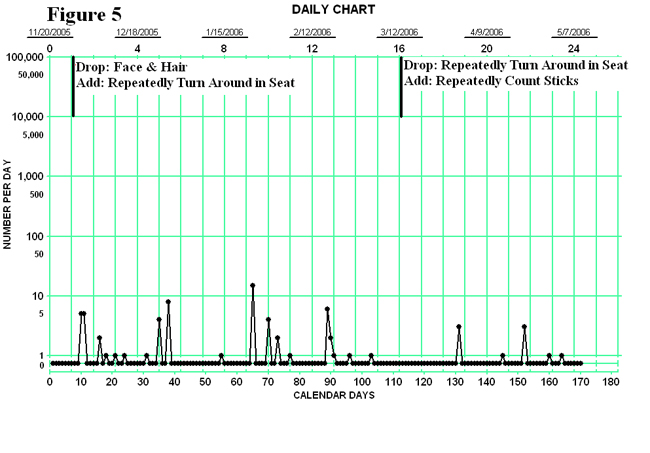
Figures 3 and 4 depict the daily data of the baseline period when rituals were defined and the subsequent period when the rituals were treated with the GED. Once the behavior was reduced to zero or near zero rates the defined ritualistic behavior was moved into the category depicted in Figure 2 and a new ritualistic behavior was operationally defined and added. As can be seen there was an immediate reduction, to zero rates in all cases. Figure 5 depicts two operationally defined rituals that decelerated as soon as she was aware they were being recorded separately and were no longer exhibited a rate that warranted more aggressive treatment.
Conclusions
Contingent skin shock was effective in reducing high rate repetitive behaviors associated with chronic Obsessive Compulsive Disorder that did not respond to over 17 years of psychiatric, pharmacological and positive only behavioral treatments.
Reduction of the behaviors increased her ability to socially interact with peers and family and actively participate in an educational program and increased access to her community.
She was able to develop rule-governed behavior and withhold some of the targeted ritualistic behaviors with just the knowledge that they were being recorded.